PORT are extremely pleased to be funding the following research project at a cost of £40,000.
Prof. Jo Martin will lead this project. PORT are proud to be in a position to fund such an important piece of research which will benefit sufferers of Pseudo Obstruction..[/lead]
P.O.R.T. – Newly discovered enzyme defect
We have been studying the structure of the bowel wall in conditions where the gut does not move properly. Patients with these gut motility problems have pain, nausea, vomiting, bloating and diarrhoea. Some are severely affected, and cannot eat, they rely on artificial nutrition and many end up having sections of their bowel removed. These patients typically have a long history of seeing many different doctors over many years, having admissions to hospital and many investigations, often without a definite diagnosis.
We have recently discovered that many of these patients have changes in a key enzyme which controls energy levels in cell, particularly in muscle cells. They have low levels of this enzyme in their blood, which means that we may be able to test for the disease very early on, get a clear diagnosis and then manage the condition in a very different way than the patients are treated currently.
We recently also have found that this enzyme is normally at a higher level in the bowel wall than in the blood, where it is usually measured, and that it is present in normal people at very high levels in the nerve cells of the bowel.
This is a very exciting new discovery in the field, but we still need to answer three very important questions:
How common is this defect in patients with pseudo-obstruction and milder forms of disorder, including abdominal pain? We have detected this change by working with samples from patients who had such severe bowel problems that they had operations to biopsy their bowel wall. We know from our control series of patients that have similar symptoms, but have not had biopsies, that many of these patients also have low levels of the enzyme ?
Can we detect these changes using simpler tests than the expensive and time consuming DNA and enzyme tests we have to use now? To test the enzyme levels and to confirm some of the changes we have to use a complicated enzyme test that needs very fresh samples and often needs retesting, as well as gene screening, which may not pick up all the changes that might be present ?
Can we find drugs or related therapies that might help boost enzyme levels and treat the condition? We know a little about some of the metabolic pathways where this enzyme works, and we still need to work out where we might be able to increase levels of the enzyme or to decrease the effects of a faulty enzyme ?
We will answer these questions by
screening patients with these conditions and related disorders such as irritable bowel syndrome, for changes in the enzyme levels.
developing a new assay for the enzyme using a special technique that breaks down proteins into its component parts, examines each fragment and compares it with the normal pattern. This is a quick, cheap and efficient technique that will give us information on the structure and the amount of enzyme.
studying the metabolic pathways that relate to the enzyme, look at databases and agents that might help alter enzyme levels. These agents will be tested initially in cells grown in the laboratory. We will concentrate first on existing agents that are already in use for other diseases, since these agents can be used in trials more quickly than other new drugs.
As soon as we have some help to gather the samples and do the testing, the first and second parts
of the work can be started immediately and will be done together, and the initial work for the third part can also be started.
We will collaborate with a number of experts in other centres across the world to make sure that we have as big a coverage as possible of all changes in the enzyme, shown in as many patients as possible. This is important in order to cover patients with a range of different backgrounds (we have some evidence that some of the enzyme changes are commoner in certain backgrounds) and also to make sure that we get as much coverage as possible for developing potential drugs.
Glycogen metabolism in the bowel wall.
Glucose is stored in cells in chains called glycogen. These chains are created by the action of an enzyme called glycogen synthase adding glucose units together (blue circles in the first picture below). As the chains form, they are made into branched structures by an enzyme called glycogen branching enzyme (Figure 2).
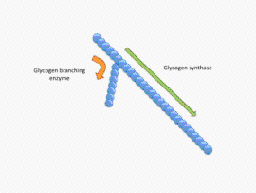
Glycogen synthase and glycogen branching enzyme work in balance together.
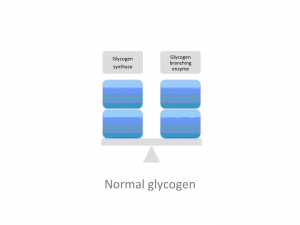
If the balance between the enzymes is disturbed so that there is a reduced branching enzyme, or increased synthase, as shown above, then long glycogen chains are produced, with fewer branches as shown in the pictures below.
If chains don’t branch they can damage the cell because the long chains are not very soluble. Since glycogen is broken down to release glucose from the ends (red circles), if there are fewer branches to glycogen, then the rate at which glucose can be released is lower, leading to problems with energy supply.
We have been looking at patients who have pseudo-obstruction in whom we found polyglucosan bodies in the muscle of bowel wall. These bodies are ovoid inclusions that stain up bright purple when looked at with a particular stain for carbohydrates. These bodies are made up of abnormal, long chain glycogen.
Glucosan bodies in muscle of the bowel wall of a patient with pseudo-obstruction
We have been looking glycogen branching enzyme in these patients, and it is low compared with normal. We have also found that a very small number of these patients have a gene defect in the enzyme that stops it working. We have tested the idea that other defects that could raise the levels of glycogen synthase can lead to the same problem in the bowel wall, and this has proved to be so.
Polyglucosan body in the bowel wall where glycogen synthase is increased.
We have also seen very high levels of branching enzyme and glycogen synthase in the normal bowel wall. This is the first time this enzyme system has been described in the bowel
The conclusion we draw from this work is that there is a very important enzyme system in the bowel wall, in which a range of defects, in different enzymes, can produce similar problems. Problems with energy metabolism can result in pain and weakness, and we think that this may be an explanation for how some of the problems in the bowel wall in pseudo-obstruction may come about.
Jo Martin
May 2012